How to Treat Dry Mouth in Older Patients
There are many diseases such as Xerostomia and Salivary Gland Hypofunction, radiation therapy in the head and neck area, and medications that cause dry mouth. In this article, we present several treatment options for older patients experiencing dry mouth.
Mouth Moisteners
Several mouth moisteners in the form of salivary substitutes or artificial saliva are available as rinses, aerosols, toothpaste, mouthwashes, lozenges, or chewing gums in the U.S. and worldwide, as shown in the table below.
| PREPARATION | PRODUCTS | ACTIVE INGRIDIENTS |
| Sugarless Chewing Gums | Biotene dry mouth gum (GlaxoSmithKline) | Sorbitol, Xylitol, Maltitol |
| Orbit (Wm. Wrigley Jr. Company) | Sorbitol, Mannitol, Xylitol | |
| Eclipse (Wm. Wrigley Jr. Company) | Sorbitol, Mannitol, Xylitol | |
| Extra (Wm. Wrigley Jr. Company) | Maltitol, Sorbitol, Mannitol | |
| Trident/Stimorol (Mondelēz International) | Sorbitol, Mannitol, Maltitol | |
| Ice Breakers (The Hershey Company) | Xylitol, Sorbitol, Mannitol | |
| Xylifresh (Leaf International) | Xylitol | |
| Spry Xylitol Gum (Spry Dental Defense System) | Xylitol | |
| Smint (Perfetti Van Melle) | Xylitol, Sorbitol | |
| Salix SST (Scandinavian Natural Health & Beauty Products, Inc) | Sorbitol, fruit acid | |
| Sugarless tablets/discs/patches | Xylimelts (Orahealth Corporation) | Xylitol |
| Sugarless solution/spray | Mouth-Kote (Parnell Pharmaceuticals, Inc.) | Yerba santa, Xylitol, lemon oil |
| Sugarless hard candy, mints, lozenges or lemon drops | Many preparations available – Trident, Spry, Smint, ACT, etc. | Sugar substitutes, citric acid, etc. |
The principal idea of these salivary substitutes is to provide a long-lasting coating of the oral soft tissues. But sprays, liquids, or gels may need to be applied frequently throughout the day (at least 3–4 times a day) depending on their adherence and/or lasting abilities.
Lozenges or pastilles may provide a more discreet and socially acceptable means of adding moisture to the mouth since their usage maybe be better hidden. However, one needs to be aware of hidden sugars in some of these products.
Most of the currently available preparations to moisten the mouth contain either carboxymethylcellulose or mucins although preparations based on hydroxyethylcellulose, poly glyceryl methacrylate, hydroxypropylmethylcellulose, glycerol, canola oil, olive oil, and linseed extract are also reported to be useful.
Sugar-free chewing gums of various types, sweetened with sugar substitutes, xylitol or sorbitol, can be used by patients during waking hours. These chewing gums stimulate salivary production by topical gustatory or masticatory action.
There is no evidence that gum is better or worse than saliva substitutes, probably because gums are effective only if there is remaining salivary functional tissue. However, chewing gums can be problematic for older adults, especially those who wear removable appliances or have arthritis affecting the temporomandibular joint (TMJ).
Lozenges or pastilles containing Xylitol that dissolve on the tongue or are adherent to the buccal surface of the tooth and are not to be chewed may give better comfort for these cases, with less likelihood of adhering to the denture component or aggravating TM joints.
Prescription Dry Mouth Medications
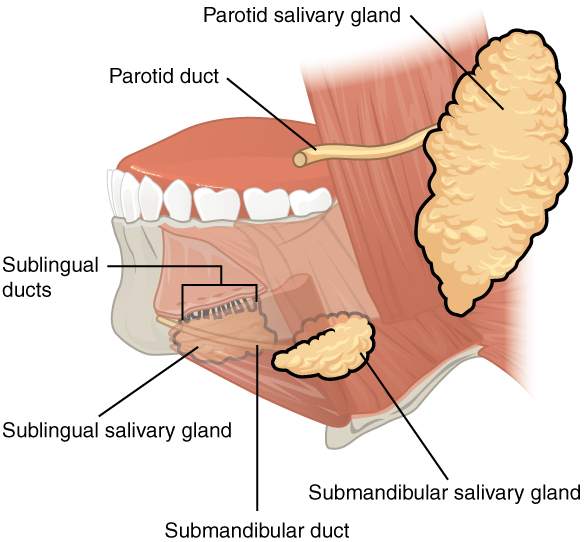
In cases when topical therapy cannot provide adequate relief of dry mouth symptoms or cannot control the complications of dry mouth, prescription-strength systemic medication in the form of sialagogues such as pilocarpine and cevimeline, orally administered parasympathetic agonists of the acetylcholine muscarinic M3 receptors, may be considered.
US Food and Administration approved these parasympathetic agonists to increase salivary secretion in patients with Sjogren’s syndrome (pilocarpine and cevimeline) and head and neck cancer patients with radiation-induced salivary gland hypofunction (pilocarpine only).
These sialagogues cannot increase the function of salivary glands that are completely destroyed, but they can enhance the function when there is residual glandular tissue.
Pilocarpine
The optimal dosage of pilocarpine 5–7.5 mg three to four times daily or 10 mg 3 times daily is generally well tolerated. Pilocarpine (SALAGEN; MGI Pharma, Bloomington, USA) should be prescribed for at least 8–12 weeks to see if there is a positive response and if long-term use would be planned due to the presence of residual salivary gland tissue that has become functional as a result of the medication.
Cevimeline
Cevimeline (EVOXAC; Daiichi-Sankyo, Tokyo, Japan) 30 mg taken 3–4 times daily, increased salivary flow, and improved subjective and objective symptoms of patients with dry mouth and is also well tolerated by patients.
Sialagogues need to be administered long-term, basically life-long since the observed clinical improvements in salivary gland hypofunction diminish after cessation of sialagogues.
Side Effects of Sialogogues
The side effects of these medications include but are not limited to sweating, increased urgency or frequency of urination, lacrimal and nasal secretion, and joint pain. Both medications, but this is true more so for pilocarpine, are contraindicated in patients with narrow-angle glaucoma, acute iritis, uncontrolled asthma, chronic obstructive pulmonary disease (COPD), kidney stones, gall stones, and heart or liver disease. Both medications can cause dehydration as well. Hence, sialagogues must be given with a high rate of caution in our older adult population.
Another systemic sialagogue of interest is Bethanechol HCL, with promising results in patients with radiation therapy-induced hyposalivation. However, further studies are needed to determine the dose, frequency of use, long-term efficacy, and safety for the use of Bethanechol.
Non-pharmacologic Interventions
Non-pharmacologic interventions for dry mouth include electrostimulation of the salivary glands with hand-held battery-operated devices or removable intraoral devices; manual and electro-acupuncture; hyperbaric oxygen therapy and application of low-level laser therapy. There is however little or insufficient evidence in the literature in definitive support of these interventions in the management of dry mouth.
Immunologically active agents such as interferon-alpha, corticosteroids, hydroxychloroquine, and other immunosuppressants such as cyclophosphamide and thalidomide have been studied for the management of dry mouth by suppressing the glandular damage from immunologically mediated diseases such as Sjogren’s syndrome and others such as sarcoidosis, HCV, and HIV infection related salivary gland diseases.
Cost Effectiveness of Treatment


Given the myriad of choices for the treatment of dry mouth, it is easy for a practitioner to be unsure as to what to recommend to a patient who has clinical signs with or without symptoms.
A cost-effective study examining the various treatments that are currently available or in development for this condition when it occurs as an outcome of head and neck cancer therapy was mounted by Saportas et al. Her group indicated that the most effective and attractive way to address dry mouth in these patients is by protecting the salivary glands from radiation damage in the first place.
To do so, changes to the conventional therapy techniques previously used must be employed. Several solutions that meet this objective are available and have demonstrated moderate effectiveness.
For example, newer radiation techniques including not only Intensity-modulated RT (IMRT), but also Intensity-modulated Proton Radiation Therapy (IMPRT), which uses protons instead of X-rays. When IMPRT is employed, reduced findings of hyposalivary function from 80% down to 25–40% have been reported.
Another protective action would be to institute the use of radioprotective drugs such as Amifostine, which has been approved for the treatment of salivary hypofunction. However, this drug does have significant negative effects such as nausea and vomiting, and its use during IMRT has been indicated as possibly unnecessary since the major salivary glands are being spared in this type of therapy, unlike in conventional radiation therapy.
Surgical procedures, including salivary gland transfer to an area outside of the radiation field (e.g., transfer of the submandibular gland to the submental space), have been shown to spare the gland and its function.
Hydration devices are also available as one of the current palliative treatments for radiation-induced xerostomia in addition to the administration of sialagogues, acupuncture, saliva substitutes, and electrical stimulation of salivary secretion.
Emerging preventive treatment solutions include systemic administration of growth factors such as insulin growth factor 1 (IGF-1) or keratinocyte growth factor (KGF) administration of botulinum toxin (BoNT), another radioprotective drug called tempo,l and the regeneration of the salivary gland tissue by gene therapy or by transplantation to the salivary gland of bioengineered salivary gland germ cells.
Even with all of these existing and emerging therapies for radiation-induced salivary hypofunction, there is a large treatment gap, and the most efficacious treatment with the most cost-effective ratio is still not available.
Solving this treatment gap will not only serve the needs of the patients with radiation-induced salivary gland hypofunction, but also will help the majority of patients who are more likely to have dry mouth from more frequently seen conditions such as medication-usage.
Conclusions
When it comes to the treatment of dry mouth conditions, either objective or subjective, there are no easy answers as to the best course of action for a specific individual.
As previously noted, there are many conditions that can cause dry mouth. While most of the cited studies have examined the most difficult cases of dry mouth, that is, those that are a result of treatment for head and neck cancer, there are many individuals who demonstrate dry mouth from far less grievous circumstances.
Taking a thorough history in an attempt to discover the contributor to and/or cause of the signs and/or symptoms and based on those findings, attempting to select the most appropriate intervention is the critical role of the practitioner. Additional factors such as patient comfort, motivation, access to the various treatments, and cost will also play a role in the selection of successful therapy.
It is important to recall that water is an essential component of life. Begin by educating the patient about possible causes of dry mouth. An analysis of fluid intake (e.g., a daily fluid diary) may be a good place to start and may also be the most practical, cost-effective, and efficient treatment with the best risk-benefit ratio.
About the Authors
The original article, “Dry mouth: A critical topic for older adult patients,” was authored by Phuu Han, Piedad Suarez-Durall, and Roseann Mulligan, Director Geriatric Dentistry Master and Certificate programs at the Herman Ostrow School of Dentistry of USC, and was originally published by Elsevier in the Journal of Prosthodontic Research.